Innovative technologies such as the diode laser have provided considerable benefit to dental patients and professionals. Facilitating efficient cutting of tissue and subsequent coagulation, the soft tissue laser enhances tissue healing and can reduce postsurgical complications. Due to the conservative nature of treatment accomplished with the laser, this technology is very useful in orthodontic procedures. The diode laser is utilized in both esthetic enhancement of the smile, and treatment management of soft tissue issues that impede efficient orthodontic treatment. Its clinical application is illustrated here in a series of orthodontic cases using the Odyssey Navigator.
For orthodontic procedures, lasers are now being used to reshape gingival soft tissues for esthetic finishing and solve issues involving altered tooth eruption. This technology is significantly and efficiently improving the design, health, and overall appearance of orthodontic patients’ smiles, while enhancing the chairside experience. Orthodontists’ interest in smile design has dramatically increased as a result of both their collaboration with dentists in interdisciplinary treatment and as the potential of laser-assisted dentistry is more readily understood by orthodontists. The 810 nm diode laser, which has numerous benefits for orthodontic treatments. It is manageable in size and low in cost. Because in most cases only topical anesthesia is necessary, the orthodontist does not need to introduce injection syringes to the patient; this is particularly beneficial in the open orthodontic clinic where siblings are often observing treatment. Additionally, patients are not burdened with the profound sensation of local anesthesia and its prolonged effects.1,2
The diode laser separates and coagulates at the same time, facilitating immediate hemostasis and resulting in minimal bleeding. Healing is rapid and there is a reduced potential for infection. Postoperative complications are minimal and sutures are unnecessary. The diode laser has an affinity for only soft tissue, thereby preventing damage to the surrounding bone and enamel—a significant advantage for the orthodontist. Finally, orthodontic procedures can be accomplished in less time and in fewer visits.1,2
Effect of the 810 nm Laser on Soft Tissue
Dental laser energy has an affinity for different tissue components. The 810 nm diode laser, for example, has energy and wavelength characteristics that specifically target the soft tissues. It has an affinity for hemoglobin and melanin, which are the components that provide color—or pigmentation— to the tissue. Other wavelengths of lasers are attracted to water, which is located at the surface of the tissue. Because the 810 nm diode laser has an affinity for hemoglobin and melanin, it is more efficient and better equipped to address deeper soft tissue problems.5-8
The light energy released by the diode laser transforms into heat, resulting in the vaporization of cells, a process referred to as the photothermal effect. The diode laser’s optical fiber is the mechanism that delivers this energy to the tissue. The degree to which the tissue absorbs this energy depends on its affinity to the laser’s wavelength, the clinician-selected energy output (which is dictated by the darkness of the tissue), the time of exposure, and the characteristics of the targeted tissue.1,3 The absorbed energy increases the temperature of the targeted tissue, immediately resulting in a sequence of tissue reactions (e.g., which ranges from warming and welding to coagulation, protein denaturalization, vaporization, drying, and carbonization depending on the amount of heat used) according to the specific desire and under the direct control of the clinician.4 resulting in a very clean surgical margin termed a biodressing.This instantaneous reaction is termed ablation. Ablation is the separation of the tissue, which results in an incision that is sealed, sanitized, and protected by a biodressing (Figure 1).
 |
This enables clinicians to modify soft tissues in a clear field without bleeding.
Whereas a surgical scalpel cuts tissue via friction, the diode laser does so through light energy that is delivered in either a continuous or pulsed mode. When used in the continuous mode, soft tissue absorbs continuous energy, thereby resulting in higher levels of heat. The more heat generated, the more postoperative discomfort may be experienced by the patient. The pulsed mode, however, allows for cooling between pulses of energy. Therefore, for soft tissue procedures, it is this author’s recommendation that the diode laser generally be used at a low power setting (e.g., 1.0 W to 1.8 W) and in the pulse mode.
The Diode Laser in Orthodontic Smile Design
Orthodontists often focus on occlusal goals, arranging the teeth in the most esthetic position possible, and then reshaping incisal edges at the end of treatment. They occasionally overlook the other elements of an esthetic smile (e.g., ideal incisal contour, height/width proportion, embrasures, contacts, gingival contour (Figure 2) that can be precisely corrected or enhanced with the soft tissue diode laser.
 |
The patient in Figure 3, for example, had undergone orthodontic treatment, but her finished smile was not as esthetic as it could be. The gingival heights of the anterior teeth were not ideal, creating an asymmetric smile. The right central incisor had a narrow gingival apex and asymmetric gingival shape, while the left central incisor had a flat gingival shape and was disproportionately short (Figure 4).
The diode laser was used to recontour the gingival shape (Figure 5); four weeks postoperatively, the patient’s smile had significantly improved (Figure 6). Precise shaping was possible due to the “tactile feedback” of the laser’s fiber. As there was virtually no bleeding, the clear surgical field enabled the clinician to easily visualize the intended tissue contour.
 |
 |
In orthodontic smile design, the method used for bracket placement depends on the needs of each individual case. For accurate bracket placement, however, the entire crown should always be visible. It is often ideal to address compromised tooth proportion prior to orthodontic bracket placement. To do so, the orthodontist first measures the amount of incisal display when the patient’s lips are at rest and in a smile. In this case, only 5 mm of the maxillary incisors were displayed in her smile due to delayed passive eruption (Figure 7). As a result of the gingival encroachment, the bracket would have had to be placed well below the center of the tooth (Figure 8), but this would result in incisor intrusion and even less tooth display on smile.
After probing the anterior teeth and taking into account the biologic width, it was determined that a gingivectomy/gingivoplasty using the 810 nm diode laser would provide adequate crown exposure to permit more ideal bracket placement (Figure 9).
Specifically, the patient would gain 5 mm in crown length and with normal reestablishment of the attachment apparatus would yield a 4-mm gain in incisal height. At the bracket placement appointment, the diode laser was used to remove the excess gingival tissue. The result was a dramatic increase in crown access and display that would permit proper bracket placement after the laser procedure (Figures 10 and 11).
The diode can also be used to finish smiles in orthodontic treatment, such as when the patient has disproportionate crown width and height (Figure 12).
The gingival margins of the patient’s lateral incisors were slightly below the gingival heights of the central incisors and canines. One treatment option was to orthodontically intrude the lateral incisors so the gingival margins more closely approximated the ideal width and height and to place porcelain veneers to restore the length of the tooth. The other option was to use the diode laser to lengthen the lateral incisors to improve tooth proportion, then to remove the brackets and re-bond them, thereby extruding the anterior teeth to more closely match the smile arc (Figure 13).
Once the Odyssey soft tissue laser was used to lengthen the lateral incisors (Figure 14), realignment was completed to enhance the esthetics of the patient’s smile (Figure 15).
Management of Altered Tooth Eruption via Combined Laser/Orthodontic Therapy
Orthodontists are under constant pressure from patients and parents to finish treatment in a timely manner. An unexpected benefit of the soft tissue laser is the ability to control tissue response due to poor oral hygiene and to remove tissue so that clinicians can access slowly erupting or even unerupted teeth.
When orthodontic patients do not follow adequate oral hygiene regimens, the removal of orthodontic appliances may result in enlarged interdental papillae and gingival margins (Figure 16).
In order to remove the enlarged papillae from this patient, the laser’s tip was wiped across the bulky tissue, and ablation reduced the bulky papillae and removed pseudopockets, facilitating improved cleaning (Figure 17).
When treating the enlarged gingival margins, the author again took advantage of the laser’s precision to shape the gingival margins against the tooth’s crown. In this case, the patient exhibited an immediate response to the laser and, approximately four weeks postoperatively, showed marked improvement (Figure 18).
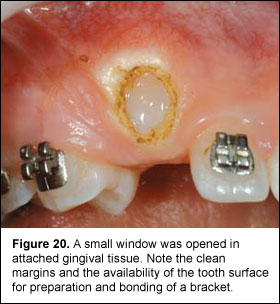
In the past, orthodontic treatment was often delayed or compromised by the incomplete or late eruption of the targeted teeth. Partially erupted teeth can be of particular concern when the clinician must place orthodontic brackets. When a tooth was partially erupted, treatment options were limited. The clinician either had to wait for the tooth to erupt through the tissue or have a periodontist remove the tissue—both of which added time to the treatment process. With the diode laser, however, orthodontists have the ability to remove the covering tissue (Figures 19 through 23).
 |
 |
 |
 |
 |
Due to the laser’s ability to immediately seal the incision with a biological dressing, the brackets could be placed on the patient in a single visit.
Additional Applications
Aphthous ulcers continue to be one of the most uncomfortable conditions orthodontic patients experience, and these ulcers can prolong treatment. There are treatments available, but most of the options do not eliminate the pain—they simply offer temporary relief. The diode laser is providing a welcome solution. With the diode laser, it takes approximately one day for the ulcer to heal and disappear. Patients are pleased because the pain from the ulcer is eliminated immediately, and the process takes a matter of minutes.
Conclusion
Diode lasers exemplify how critical technology is in modern dentistry. As clinicians are becoming more knowledgeable about the benefits of laser use in therapy, they are growing more comfortable with applying lasers to several different procedures. Whether orthodontists are correcting excessive gingival display or aiding in crown lengthening, laser technology is dramatically increasing the level of care to patients. Not only are lasers making a practice more effective and efficient, but they are also providing a more comfortable patient experience.
References
1. Rossmann JA, Cobb CM. Lasers in periodontal therapy. Periodontol 2000 1995;150-164.
2. Sarver DM. Principles of cosmetic dentistry in orthodontics. Part 1. Shape and proportionality of anterior teeth. Am J Orthod Dentofacial Orthop 2004;126:749-753.
3. Research, Science and Therapy Committee of the American Academy of Periodontology. Lasers in periodontics. J Periodontol 2002; 73:1231-1239.
4. Sarver DM, Yanosky M. Principles of cosmetic dentistry in orthodontics. Part 3. Laser treatments for tooth eruption and soft tissue problems. Am J Orthod Dentofacial Orthop 2005;127:262-264.
5. Miyasaki MA. Shedding light on the soft tissue laser. Signature 2004;11(1):11-13.
6. Patino MG, Neiders ME, Andreana S, et al. Collagen. An overview. Implant Dent 2002; 11(3):280-285.
7. Patino MG, Neiders ME, Andreana S, et al. Collagen as an implantable material in medicine and dentistry. J Oral Implantol 2002; 28(5):220-225.
8. Patino MG, Neiders ME, Andreana S, et al. Cellular inflammatory response to porcine collagen membranes. J Periodontal Res 2003;38(5):458-464.